Drug prevention
The Icelandic Model
(Planet Youth)
The issue of alcohol and drug misuse is of major concern in Northern Ireland.
The Icelandic approach to effective, evidence-based prevention in the field of alcohol and other drugs is based around a detailed questionnaire completed every two years by every school child in Iceland aged between 10 and 20 years old.
The survey asks questions about

The data identifies the factors that are having a negative impact on young people making them more likely to use alcohol and other drugs (risk factors) and the factors that are having a positive impact making young people less likely to use alcohol and other drugs (protective factors). Although the situation varies between countries and cultures, the main protective factors for young people are universal: children’s relationship with their parents and involvement in good quality organised activities.
The Background
20 years ago in Iceland, the young people there had the highest level of alcohol and drugs use across Europe.
Despite a concerted approach to
The multi-agency team focused on increasing adolescent participation in structured and
Results
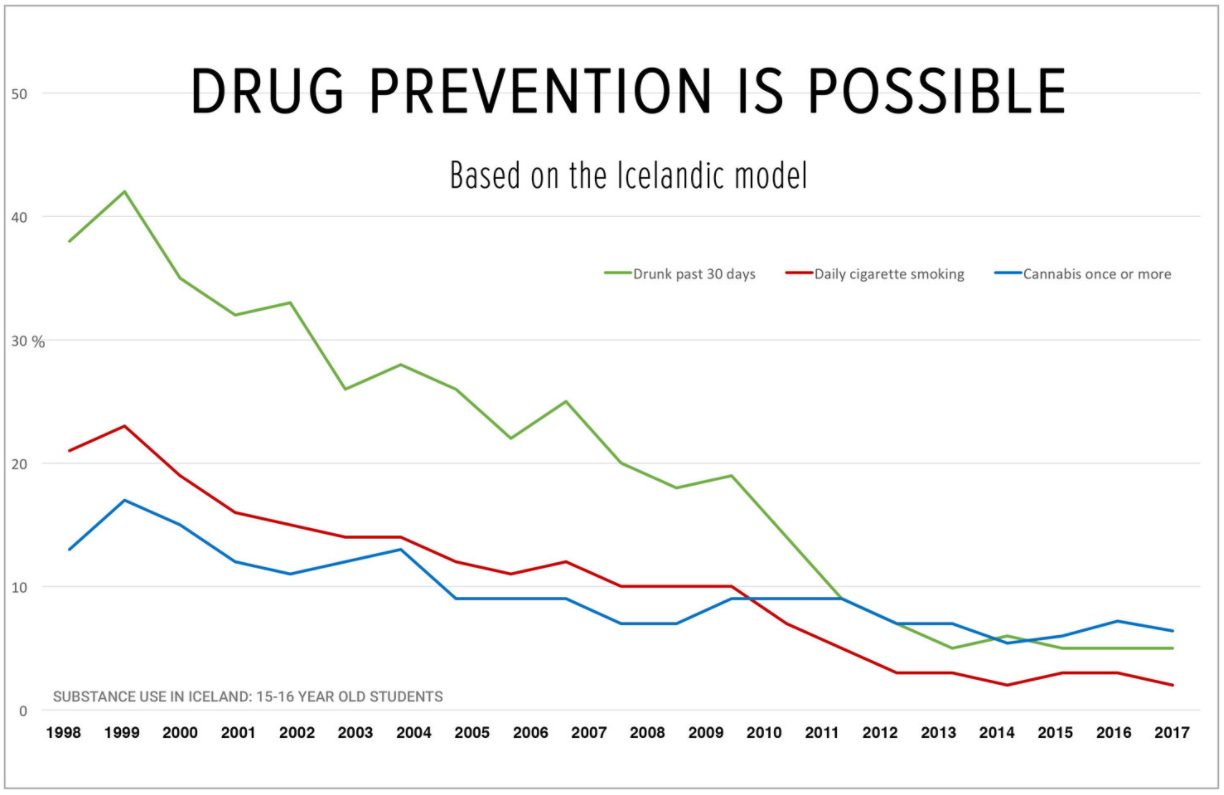
This graph shows the decline in alcohol, smoking and cannabis use in young people aged 15-16 years old in Iceland.
All the agencies involved with
What type of changes did they make in Iceland?
In the city of
A lot of work has gone in to supporting parents and encouraging them to spend more time with their children. According to Jón Sigfússon, the Director of Youth in Iceland at the Icelandic Centre for Social Research and Analysis (ICSRA), “Parents are the biggest preventative factor in children’s lives”.
In Iceland, parents sign up to a ‘Parental Contract’ which sets out rules for both parents and children about spending time together, rules about children’s drinking and drug-taking and the time children must be home. On a government level, Iceland restricted the availability of alcohol and introduced minimum unit pricing. These are a few examples of the type of interventions adopted by Iceland since the model was introduced in 1997.
Young people in Iceland do not receive any drug education as part of this initiative. When asked about this Jón
But what about Northern Ireland, would it work here?
As of 2019, the Icelandic team has worked with 110 communities in 27 countries across the world to implement the model as part of what is now called the ‘Planet Youth’ initiative (visit www.planetyouth.org for more info). Each of these countries, towns and cities has a unique set of circumstances and challenges. Whilst the survey remains relatively static, the interventions in each country are carefully tailored based on those survey results, and so the approach is highly adaptable and also effective.
What next?
There appeared to be broad support for this approach. The Chief Medical Officer, Dr. Michael McBride, tasked the Public Health Agency with considering the viability of implementing the approach in Northern Ireland. Conversations have been ongoing with relevant stakeholders such as Dept of Health, Dept of Education, Dept of Justice, Dept for Communities as well as representatives from local councils, local health trusts and the Education Authority.
More recently
The Advisory Council on the Misuse of Drugs have since made recommendations to UK government (see in particular 3.8).

Talk to someone, you are not alone.
Lifeline counsellors are available 24 hours a day, seven days a week to listen and help, in confidence.
Deaf and hard of hearing Textphone users can call Lifeline on 18001 0808 808 8000. Calls to Lifeline are free to people living in Northern Ireland who are calling from UK landlines and mobiles.

Something went wrong with the twitter. Please check your credentials and twitter username in the twitter settings.
Problem displaying Facebook posts.


